Written by
Maurice M. Garcia, M.D., MAS
Assistant Professor
Department of Urology
Cedars-Sinai, Los Angeles, CA
THE HINMAN YEARS: 1915-1950
The discipline of urology at the University of California San Francisco is relatively young. Other institutions led the way, among them Johns Hopkins, Columbia, Harvard, and the University of Pennsylvania.

The first mention of the specialty at UCSF dates to 1900 when Dr. John Williamson, a UC graduate of 1885, was listed as Professor of Anatomy and Genitourinary Surgery. At this time there was no University Hospital. Most of the patients were seen in the out-patient clinic downtown on Montgomery Street, and all surgery was performed at San Francisco County Hospital. In 1902 the curriculum listed 36 hours of demonstration clinics in genitourinary diseases and 108 hours of practical clinics. In 1912 Dr. William B. Willard was appointed an instructor in urology and took charge of the Outpatient Department. Senior students then had 11 hours of lecture and 40 hours of section work in urology. In 1915, the Division of Urology was established when Dr. Howard C. Naffziger, Chairman of the Department of Surgery, appointed Dr. Frank Hinman, Sr., as its Chair.
Frank Hinman, Sr.
Dr. Frank Hinman, Sr. was born in Forest Grove, Oregon, to a pioneer family on April I, 1880. In 1902 he graduated from Stanford University, where he edited the campus newspaper, The Stanford Daily. For medical school he chose Johns Hopkins where William Osler was still professor of medicine and Welch, Halsted and Kelly were developing the pattern for modern medical education.
He graduated in 1906 and returned to the Northwest to pursue general practice in Spokane. However, his partial deafness from old mastoiditis made this impractical and he returned to Hopkins for training in Urology under Hugh Hampton Young. He was Chief Resident when the newly completed Brady Institute opened. After finishing his training in 1915, he returned to San Francisco where he was appointed to the teaching staff at the University of California and, shortly thereafter, became responsible for the Urology Division.
In those days, the first two years of medicine were taught on the UC Berkeley campus. With Dr. Hinman's appointment as Chair, he secured a small comer office on the 4th floor of the old University Hospital to serve as the Division's headquarters (in marked contrast to the thousands of square feet that the Department occupies today). There he had room for a desk for himself and one for his editorial secretary, Mrs. Anne Green.
Besides being an outstanding clinician, Dr. Hinman was a scientist at heart. Whenever he faced a problem in his clinical practice, his mind immediately shifted to the research lab. His broad research interests covered diverse topics: hexamethylenamine, priapism, the waxed-tipped catheter, renal and prostatic (perineal) operative techniques, radical surgery for testicular tumors, renal counterbalance, pyelovenous back flow, operative treatments for megaureter, gonadotropins in testicular cancer, and many others. His great contribution, however, was his monumental work, The Principles and Practice of Urology, first published in 1937. In this he was assisted by Mrs. Green, whose training as a librarian proved invaluable. She not only prepared the manuscript, but also (with a primitive 35-mm camera) photographed illustrations from articles in the library that were to be incorporated. Ralph Sweet, the outstanding medical illustrator, provided the original drawings.
Dr. Hinman was a member of many medical societies. Besides being a Fellow in the American College of Surgeons, he was a member of the American Medical Association, American Urological Association, Association of Genitourinary Surgeons, Clinical Society of Genitourinary Surgeons International Association of Genitourinary Surgeons, and the Societe Francaise d'Urologie (Corresponding Member). Dr. Hinman took seriously his obligation to these medical societies. In 1927 he was the Chairman of the Section of Urology of the American Medical Association; in 1937 he was elected President. In 1940 he was elected President of the Clinical Society of Genitourinary Surgeons, and was also awarded the prestigious Keyes-Medal by this society in 1954.
In 1948, Dr. Hinman was 67 years old, the normal retirement age according to university policy. However, the sudden death of Dr. Clark Johnson, his planned successor, prompted Dr. Francis Scott Smyth, the Dean of the Medical School, to write a letter to the President of the· University, Dr. Robert Sproul, requesting an exemption. President Sproul obliged and Dr. Hinman's chairmanship was extended to June 30, 1950, when he retired at age 70.
Because Dr. Hinman had been accustomed to operating two mornings a week and working in the office the alternate three afternoons, this schedule had allowed him time to pursue his other interests throughout his career and made the shift into retirement relatively easy. He and his wife (the former Mittie Fitzpatrick) had a country home in Woodside, near Stanford, 40 minutes south of San Francisco, where he raised horses and rode the country trails. Before retirement, he had become interested in methods of keeping older people active and had worked with Stanford to establish the field of gerontology. However, after retirement, when he found he had plenty to occupy him, he lost all interest in the field. Instead, with the aid of his many professorial friends at Stanford, he wrote and published The Impact of the New Physics.
Heart block from old rheumatic mitral disease caused his death in 1960, at the age of 80. .In his eulogy to the Genitourinary Surgeons, Dr. Charnock wrote: "His passing thins the ranks of those pioneers who elevated Urology to the high scientific standing we enjoy today. This Association has lost a respected member. The profession has lost a gifted physician. Those of us who were privileged to serve under him have lost a true friend."
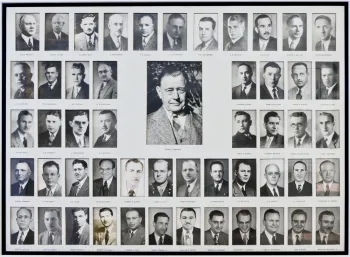
The Program. When Dr. Hinman became Chief of Urology at UC-SanFrancisco, urology at large was a new specialty. He established a rotation for residents (see Figure 2) among the University Hospital (6 to 8 beds), FranklinHospital ([now Ralph K. Davies Medical Center], a private hospital with 10 to15 available beds), and the San Francisco County Hospital (later San FranciscoGeneral Hospital), where Stanford and UC shared a large open ward of some30 beds.
A volunteer faculty did all the resident and student teaching, with Dr. Hinman's associates covering most of it, especially at the County Hospital. Here, in contrast to the private Franklin Hospital, the resident took charge of patient care. A shortage of beds at UC Hospital led Dr. Hinman to move his private practice and that of his associates to Franklin, where the residents often would assist the attending physicians or be allowed to perform the procedures under strict supervision. The UC Hospital service was smaller, but it received more unusual problems and had a small but active pediatric service.
It was the custom for many years for a junior resident to spend one afternoon a week at the "pee bench" in Dr. Hinman's private practice office in the Fitzhugh Building on San Francisco's Union Square. His duty was to take the patient's history, collect and analyze the urine samples (including a methylene blue smear of every specimen), and perform a PSP test (phenolsulfonphthalein; now historic) for renal function and residual urine. It was here that residents would pick up the rudiments of office practice before going out on their own.
When the program was in full operation, two or three residents would start each year and spend a total of three years in clinical urology. Work in the laboratory was fitted into the clinical schedule. Prominent graduates from his program include Elmer Belt, T. E. Gibson, W. A. Carroll, Justin Cordonnier, Tracey Powell, Donald R. Smith, Robert G. Weaver, Bill Smart, Mathew Marshall, Stanwood Schmidt, and Frank Hinman, Jr..
Anecdotes from his residents abound. Dr. Stanwood Schmidt, in remembering the days of his residency (1944 to 1948), writes: “When I was a resident, Dr. Hinman had finished his research on hydronephrosis and this extensive work became a thing of the past. However, he got me to find a marine fish with an aglomerular kidney and to keep it at the Steinhart Aquarium and ligate one of the ureters to see if the kidney became hydronephrotic (of course, it did not). For a time, I was the world's greatest (and worst) fish surgeon. I later, however, wrote up this work and it was given the McCarthy Award. That experience made research fun for me and I continued to dabble in it even in my private practice in Eureka.”
Dr. Richards Lyon reminisces: “My memories of "Pop", as we called him behind his back then (always with great respect, even reverence), are suffused with an over-riding aspect of personal character-integrity. Let me illustrate the Hinman qualities and beliefs as I experience them on a day-to-day basis. I’ll start with the ‘eight steps’: 1) overall history; 2) urologic history; 3) abdominal examination; 4) genital examination; 5) rectal examination; 6) three-glass urine examination; 7) psp test for renal function; and 8) KUB. In case presentations, the "eight steps" were to be described without suggesting a likely diagnosis. Should the resident make the mistake of letting his ego drive him into early diagnosis--even though this diagnosis would eventually turn out to be correct-Dr. Hinman's abrupt comment would be ''Next case." The resident would get the message: “Pop was not interested in smart diagnoses. He knew that such are only acceptable if arrived at by disciplined work-up and that the smart diagnosis becomes the obvious diagnosis once the groundwork is laid. There was an immense pride and esprit among all his residents through the years to the point that, as we met in later life and discussed a urologic problem, the rules of work-up were so ingrained and trusted that the deciding points were quickly made. This had something to do with his determination that his residents would consider his example as just the start of a productive, ever-broadening knowledge.”
Clinical Faculty. During Dr. Hinman's tenure as Chair, many prominenturologists worked with him: Clark Johnson, his second-in-command;Henry Weyrauch, who later became Professor and Chair of Urology atStanford; and Donald R Smith, who succeeded Dr. Hinman. Other clinicalfaculty were Fred Howard, Lionel Player, Lloyd Reynolds, John Schulte,Sidney Olson, William Carroll, William Murphy, Mark Hand, Tom Gibson.
THE SMITH YEARS: 1950-1976
Donald R. Smith
Donald Ridgeway Smith, who succeeded Dr. Hinman as Chair in 1951, was born in Berkeley on May 23, 1909. His father, Wilfred Joseph Smith, had come to San Francisco as a volunteer during the Spanish-American War; his mother, Ethel Rosemont Smith, was of Welsh extraction. Don went to school in Berkeley, attended University High and graduated from UC Berkeley in 1931 with Honors in Medical Sciences. Dr. Smith received his M.D. from UC San Francisco in 1935, remaining to complete his internship and residency under Frank Hinman, Sr. In 1940 he joined the UCSF staff as a clinical instructor. Over the next ten years he rose in the ranks to succeed Frank Hinman, Sr. as the Chair of the Division.
His major clinical interests were fluid and electrolyte balance, renal physiology, reconstructive surgery (especially hypospadias repair), urinary tract infection, and pediatric urology. Shortly after assuming the chairmanship he devoted two years to putting together his now well-known textbook, General Urology (Appleton and Lange). This book, now in its fourteenth edition, has become a classic for both undergraduates and practitioners.
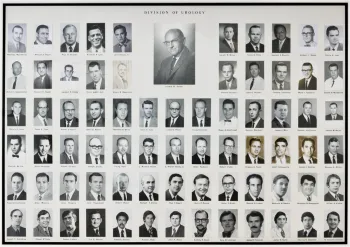
During his tenure, Donald Smith trained 72 residents (Figure 3) - all outstanding clinicians. In a recent letter, Dr. Clair Cox wrote: My easiest recollections are Saturday morning rounds at the University with Dr. Smith and subsequent coffee; working in the dog lab with Dr. Hinman; long discussions with John Hutch while dissecting a cadaver bladder; Dr. Schulte teaching me perineal prostatectomy; spending hours placing a suture line for a pye1plasty with Bill Smart. All of my memories of San Francisco and the University are pleasant. I cannot recall a single unpleasant occurrence.” This statement reflects the consistent feeling of the residents trained by Don Smith.
The Program. Under Dr. Smith's Chairmanship; the division continued to grow in stature. The faculty numbered 32, all clinical (unpaid). The three main hospitals served now encompassed UC (Moffitt Hospital), San Francisco Veterans Administration Hospital (Fort Miley), and San Francisco General Hospital. The three residents each year rotated to each of the hospitals for four months during each of the three years of training. (Added to this rotation was the old Southern Pacific Hospital [and, after the SP closed its doors, Kaiser Oakland], through while the residents rotated for four months during their second clinical year to get a taste of practice outside the university setting.) There was no specific assignment in the research lab, but all were encouraged to participate and to contribute to the literature.
All teaching of medical students was carried out by the 32 clinical faculty. Undergraduate teaching included 7 hours of lecture in the third year and 6 hours of clinical work plus 14 hours of seminars and 16 hours of both ward rounds and case presentations. In the fourth year, elective urology was available in one of the three hospitals.
Clinical Faculty: With a keen clinical sense Dr. Smith surrounded himself with distinguished clinicians: Dr. John Hutch is considered the father of vesicoureteral reflux; indeed, in 1958 he wrote a monograph on the ureterovesical junction. He was the first to develop a serious technique for repair of vesicoureteral reflux, which opened the door for a more refined understanding of the pathophysiology of this. problem. A second interest was the anatomy, physiology, and embryology of the lower urinary tract, especially the bladder outlet and the base plate as he described it. He was an original thinker, and his death in 1972 at age 50 was a great loss to the field.
Dr. William Smart had had his training under Frank Hinman, Sr. and was the last Vice-Chairman under Dr. Smith. His main contribution to urology was in the field of ureteropelvic junction obstruction and pyeloplasty; indeed, he wrote an exhaustive chapter on the subject in the early editions of Campbell's Urology. The AUA Film Library enlisted his expertise in reviewing all films dealing with ureteropelvic junction obstruction and then assigned him the responsibility of producing the necessary films to demonstrate the techniques of surgical correction, a task that was close to his heart. He devoted more than three years to this classic series, The Practice of Urology. Dr. Smart died at the age 63 on October 9, 1977.
Dr. Frederick Howard was the Chief at the Veterans Administration Hospital and Vice-Chairman of the Department from 1967 until his death in 1972. His areas of interest were infertility and intersexuality, and in 1948 he wrote the classic description of the relationship between the size of the prostatic utricle and the degree of hypospadias. His national and international reputation as an expert on intersexuality and congenital mal - development of the genitalia led to his selection to cover this topic for the Encyclopedia of Urology.
Dr. James Ellliot was Chief of Urology at the Veterans Administration Hospital in Oakland. Among his interests were metabolic disorders and renal stone disease. He applied the principles of quantitative chemistry to uncover the chemical factors in urine responsible for the development of calcium phosphate or calcium oxalate stones. He also had an interest in chemotherapy for urologic cancer and was a participant in the Veterans Administration Cooperative Study for Carcinoma of the Prostate and a member of the Pacific Veterans Administration Cancer Chemotherapy Study, which at the time was testing new chemotherapeutic agents in patients with inoperable carcinomas of the genitourinary tract
Dr. Alex Finkle had long-term experience in laboratory research and studied the physiologic responses consequent to reducing renal mass by resecting 75% of renal tissue. He also studied the alteration in renal blood flow during experimentally induced hydroureteronephrosis. He had a special interest early on in human sexuality and compared the incidence of erectile dysfunction after perineal, suprapubic and transurethral prostatectomy.
Dr. Patrick McLin is credited with popularizing office bacteriology by introducing a simplified urine-culture assessment technique that later was adopted by many practicing urologists.
Dr. Stanwood Schmidt has achieved international recognition for the success of his vasectomy technique (section-fulguration-fascial interposition). His series of 6248 patients is the second largest in the world literature.
Dr. John Schulte, Vice-Chairman of the Department and Chief of the Urology Service at Veterans Administration Hospital in San Francisco, trained under Dr. Hinman from 1942 to 1945 and then joined him in private practice. He was an outstanding clinician who was always described as having the fine combination of personal integrity, pleasing personality and excellent professional competency, which made him a teacher of the- highest order. Perineal surgery, especially perineal prostatectomy, was his forte, and we all at UCSF owe him the opportunity to learn this anatomical approach to the prostate. One of his most valuable contributions to clinical urology was the introduction of the methylene blue stain to urine sediment to detect malignant transitional cell tumors of the urinary tract. He was so revered for his teaching excellence that, after his death in 1967, Dr. Smith established a Visiting Professorship in his name (see Table 2).
Dr. Richards P. Lyon began his residency training with Frank Hinman and completed it with Don Smith, whereupon he was invited to join the clinical faculty. He soon made a name for himself as one of the field's original thinkers, and the years have not diminished his creativity. He was the first to think of compression stockings to speed up blood flow in the deep venous system, this avoiding venous stasis and embolism. However, it was his interest in fluid and electrolyte balance, supported by his background as an engineer, that inspired some of his greatest work. He proposed a bedside scale to weigh the patient postoperatively to determine blood loss and fluid shift in the extracellular space. With the creation of the standard of a half-pound weight loss per postoperative day, acute tubular necrosis became readily detectable. Patients who might previously have been lost could then be managed conservatively and saved. His syllabus on fluid/electrolyte balance has had significant impact on residency training at
UCSF. The culmination of this work has been his development of a state-of the-art operating-table scale to monitor fluid shifts. When used during TURP, the Lyon surgical scale permits resection of far larger glands than could be attempted in the past.
Frank Hinman, Jr.
Dr. Frank Hinman, Jr., a world-renowned leader in urology, has always been a major contributor to the program at UCSF. He attended Stanford University, graduating magna cum laude in 1937. He completed his medical degree at Johns Hopkins, where he finished first in his class and went on to Cincinnati for a surgical residency under the master surgeon Mont Reid. After serving two years in the Pacific on the aircraft carrier Intrepid during World War II, Dr. Hinman began his urologic residency at UC under his father's chairmanship. Finishing training in 1950, he joined his father's office and worked with him until his father retired from practice three years later. In the meantime, he joined the faculty at UC as a Clinical Instructor and progressed to Clinical Professor in 1962. He was Chief of the Urology Service at San Francisco General Hospital from 1958 to 1977 and Chief of Service at Children's Hospital from 1959 until 1985.
Dr. Hinman's broad interests cover many segments of urology: urinary tract infection, urodynamics, pediatric endocrinology, benign prostatic hyperplasia, and operative urology are only a sampling of his numerous areas of expertise. His early interest in pediatric endocrinology led him in 1951 to become one of eight founders of the Society for Pediatric Urology, which he served as President in 1961 and 1973. This interest also sparked his starting the Endocrinology Group in 1957, which in 1965 evolved into the Endocrine Forum held yearly at the annual meeting of the AUA. His interest in urodynamics, stemming from original studies begun in 1954, resulted in the publication of Hydrodynamics of Micturition in1971 from a workshop he coordinated. Subsequently, with Saul Bayarski and Jack Susset, he organized the Urodynamics Society and was its second President. He was a founding member of the Society of University Urologists, and was subsequently elected its President. In the American College of Surgeons, Dr. Hinman was elected Regent and Vice-Chairman of the Board of Regents and then Vice-President of the College. As a former member of the Resident's Review Committee on Urology, he served a six-year term on the American Board of Urology with special interest in authorization of sub-specialization.
Always curious about how things work, Dr. Hinman was an inventor with three patents. He was also an accomplished painter, and an avid sailor. His studies on the bladder defense mechanism, pediatric bladder dysfunction, and the non-neurogenic, neurogenic bladder are classic. (Indeed, the last bears his name [the Hinman Syndrome].) Although he was a prolific writer while in active practice, publishing in excess of 250 papers and the volumes Benign Prostatic Hypertrophy and Hydrodynamics before 1985, after his [so-called] retirement he produced works that have become standards in their field: Atlas of Urologic Surgery, Atlas of Pediatric Urologic Surgery, and the Atlas of Urosurgical Anatomy.
THE TANAGHO YEARS: 1976-1996
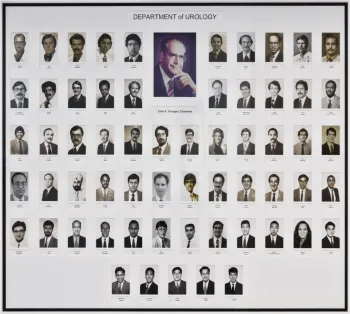
Upon the retirement of Don Smith in 1976, Dr. Emil A. Tanagho became Acting Chairman. After successfully negotiating departmental status for what had previously been a division of the Department of Surgery, he accepted the chairmanship officially.
His goals were to maintain the excellence of the clinical training while introducing a strong academic program. To the latter end, he expanded the residency from 5 years to 6, with one year devoted to research.
After being the only full-time faculty member in the department for over ten years, Dr. Tanagho charted priority plans for recruitment of full-time faculty to encompass the diverse subspecialties within the field.
Full-Time Faculty
In July 1977, he recruited Dr. Jack McAninch to be Vice-Chair and Chief of Service at San Francisco General Hospital. With his great interest in urologic trauma, Dr. McAninch integrated the residency program into SFGH's renowned Trauma Center. Indeed, Dr. McAninch has served as Chief of the Medical Staff at SFGH (1983 - 1984). In addition, he has been an active participant in our specialty societies at all levels, serving the Western Section of the AUA (President from 1991 - 1992), the American Board of Urology (President-Elect, 1995 - 1996), the Society of Genitourinary Reconstructive Surgeons (President, 1993 - 1994), the American Association for Surgery of Trauma (Vice President, 1992 - 1993), the SID (Secretary-Treasurer of the U.S. Section, 1991 -1999). In 1996, he will assume the Presidency of the AUA.
Dr. McAninch's large and on-going series of patients with renal trauma has resulted in many innovative recommendations for diagnostic efficiency and effective reconstruction. His repair of genitourinary injuries, including gunshot wounds, is highly regarded world-wide. In his work on extensive urethral strictures, he has demonstrated the success-for this very problematic injury-of his fasciocutaneous penile flap technique.
In 1978, Dr. Tanagho recruited Dr. Edwin Mears to be Chief of Urology at the Veterans Administration Hospital. However, the following year his old institution, Tufts University, recruited Dr. Mears back as Chair. In 1979, Dr. Richard Williams from the University of Minnesota succeeded him at the VAH. Dr. Williams played a substantial role in strengthening the service, combining his clinical expertise as a urologic oncologist with a growing laboratory research program. However, in 1985 Dr. Williams was recruited to chair the Department of Urology at the University of Iowa. Dr. Perinchery Narayan succeeded him and served as Chief of Service at VAH (now called the Veterans Administration Medical Center [VAMC] for nine years, leaving in 1994 to assume the chairmanship at the University to Florida in Gainesville. Dr. Joseph Presti, Jr., who completed his residency with us in 1989 and subsequently served a three-year fellowship at Memorial Sloan Kettering Cancer Center, became Chief of Service at VAMC until he was recruited to Stanford University.
In 1979, Dr. Richard Schmidt, after spending two years in Dr. Tanagho's lab, was recruited as a major contributor to the field of neurourology and urodynamics. In 1993, he left to join the faculty at the University of Colorado at Denver. In 1994, Dr. Sherif Aboseif, a UCSF resident who had spent three years in our research laboratory, replaced him.
In 1982, Dr. Tanagho recruited Dr. Barry Kogan to head the pediatric urology service. Before coming to the Department, Dr. Kogan completed a prestigious fellowship under Mr. J. Herbert Johnston at the Alder Hay Children's Hospital in Liverpool. He has a special interest in gastrocystoplasty as well as in laparoscopic surgery for non-palpable testes and has accumulated a large series of retrograde endopyelotomy patients. His research activities include the development of a unique fetal model (for which he was awarded the Grand Prize in the Jack Lapides Essay Contest in 1988), which lends itself to studies of the physiology of the lower urinary tract as well as of the congenital anomalies of prune belly syndrome, cryptorchidism, and renal dysplasia. Indeed, Dr. Kogan's reputation and industry very quickly led this subdivision to a level where a second full-time faculty member was needed to share the heavy clinical and academic load. In 1993, Dr. Laurence Baskin, one of our former residents who spent two years in Philadelphia with Dr. John Duckett, joined the pediatric urology group.
Dr. R Dale McClure was recruited in 1982 to head andrology and male infertility. He developed a busy andrology service and established an ongoing research effort in cooperation with the Department of Obstetrics and Gynecology and Reproductive Sciences. Dr. Paul Turek was recruited to head efforts in andrology and infertility when Dr. McClure left for the Virginia Mason Clinic
Also in 1982, Dr. Tom Lue, the Ferdinand C. Valentine scholar (New York Academy of Medicine), was recruited to the full-time faculty. He brought to our laboratory a strong interest in neurophysiology and erectile dysfunction, and he has since put UCSF in the forefront of the field of impotence research. Through his investigations he has elucidated the anatomical mechanism of erection- and detumescence, detailed the penile architecture, and identified the site and course of the erectile nerves. He has also developed an accurate test for penile arterial and venous function, simplified the correction of Peyronie's disease, and refined surgery for penile venous leakage. His research has been recognized with (among other awards) the Gold Cystoscope Award (1988), the AIken Prize (1987), the Jean-Francois Ginestie Prize (First Prize, 1992; Second Prize, 1986), and the Jack Lapides Prize (Grand Prize, 1994 and 1995; Second Prize, 1992). Dr. Lue has lately turned his interest to the development of an animal model for female ' stress incontinence.
In the area of stone disease, Dr. Robert Kahn, one of the residents was recruited. He had obtained further training in endourology at the prestigious Mainz University. He served on our full-time faculty for three years, from 1982 to 1985, when we acquired the lithotriptor. Professor Joachim Thüroff from Germany then served as the Director of the Stone Center for two years. He was followed by Dr. Marshall Stoller, our current full-time endourologist. Dr. Stoller is investigating a class of drugs, bisphosphonates, which have demonstrated tremendous potential for improving diagnostic capability, thus directing more efficient therapy and possibly reducing stone recurrence.
In 1986, Dr. Peter Carroll, a graduate of our program, returned from a two-year fellowship at Memorial Sloan-Kettering Cancer Center. During his fellowship, Dr. Carroll had examined cytogenetic abnormalities in urologic cancers and was one of the first investigators to identify loss of chromosome region 3p in sporadic renal cell carcinomas. He organized the Urologic Oncology Multidisciplinary Faculty Practice, a collaborative effort of the Department of Urology and Division of Medical Oncology.
The department has always cooperated with other departments in the school of Medicine, and has had on its faculty many joint appointees: Dr. Brian Mayall, Professor of Laboratory Medicine; Dr. Gerald Cunha, Professor of Anatomy; and Dr. Hedvig Hricak, Professor of Radiology who ultimately assumed the position of Chair of Radiology at Memorial Sloan Kettering Cancer Center.
Besides the full-time faculty, the program was assisted by 59 clinical faculty at various ranks who contributed significantly to our clinical activities and teaching. Noteworthy among them was Dr. Eugene Cattolica, past Chief of Urology at Kaiser Permanente in Oakland, with whom our residents rotated (until 2004) for a 4-month period during training. He was assisted by Drs. Robert Klein, Kenneth Rankin, Charles Turzan and Mark St. Lezin, all of whom are former graduates of our residency program and are outstanding teachers.
Emil A. Tanagho
Dr. Tanagho, a native Egyptian, was born on August 12, 1929. He received his medical degree from the University of Alexandria in January 1952. After obtaining his Master's degree in General Surgery, Division of Urology, he was appointed Lecturer in Urology at that institution. In 1962 he spent a sabbatical term at the University of London, Institute of Urology. He came to the University of California, San Francisco, as a research urologist from February 1963 to August 1964, and then returned to the University of Alexandria as an Assistant Professor. Discouraged with the political climate in Egypt at that time, he accepted a position as Visiting Professor at the American University of Beirut until emigrating to the United States in August 1966. He was appointed to the full-time faculty as Assistant Professor of Urology in 1967, Associate Professor in 1970, and Professor in 1972. In 1976, he became Acting Chair of the Division of Urology and Chairman of the Department when departmental status was awarded.
Dr. Tanagho's research activities covered a broad base of urologic pathology. He built upon his basic work at the Institute of Urology in London where he elucidated the anatomical structure and 'physiologic function of the ureterovesical junction and bladder neck, using 'a pioneering technique of dissection under magnification and following the anatomy by tracing muscle bundles rather than muscle fibers. At UCSF, his multilateral physiologic studies constituted the first comprehensive investigation of the physiology of this vital segment of the lower urinary tract. Dr. Tanagho then embarked on the study of the anatomy of the bladder neck and of the urethra, specifically of its sphincteric mechanism, establishing the proper anatomical morphology of the urinary sphincter.
Subsequently, his cinefluoroscopy and multiple simultaneous pressure recordings provided clear insight into the basic mechanism of interaction between bladder and urethral sphincter. This work was followed by the development of a comprehensive means of urodynamic study for evaluation of the lower urinary tract-a method that has been applied to a variety of urologic disorders and has made UCSF the leading "institution for the evaluation and understanding of such problems. Clinical application ensued, mainly a new surgical technique for the repair of total urinary incontinence by sphincteric reconstruction, utilizing specific segments of the bladder wall-first done in 1970. This has become the classic technique applied by many institutions for correction of total urinary incontinence, especially after prostatectomy.
Dr. Tanagho had (and continues to have) a lasting impact on the residents and fellows he helped train. As Dr. Marshall Stoller, a resident and then faculty member during Dr. Tanagho’s tenure as Chair, reminisces: “ I arrived in San Francisco in the early 1980's as an eager new urology resident. In the relatively small urology Department of UCSF, Dr. Emil Tanagho was exploring the use of neural stimulation for the treatment of pelvic floor dysfunction. Although I was unaware such therapies were even within the domain of urology, Dr. Tanagho was convinced that the pathology of urologic diseases could best be understood through a thorough knowledge of the relevant anatomy. This understanding of anatomy and pathology was the key, he believed, to developing novel approaches to heal our patients.
Dr. Tanagho's laboratory was located on the top floor of the Health Sciences East building. At the end of the operative day, residents and fellows gathered around the meticulously-wrapped cadaveric prosections and performed detailed abdominal and pelvic dissection to better understand neural innervation and anatomy of the pelvic organs. The knowledge and experience gained among the formalin-soaked rags of the cadaveric lab ultimately led to the use of neuro-stimulation performed via sacral laminectomy. During these early procedures we took off our patients' socks to observe the plantar flexion of the toes that occurred with stimulation of the appropriate sacral nerves. These early experiences, spurred by Dr. Tanagho's curiosity and encouragement, led me to explore other nerve stimulation techniques and culminated in the development of the SANS device (Stoller Afferent Nerve Stimulator).
After residency I was fortunate to be offered an academic post in our Department by Dr. Tanagho. In the early years of my tenure he encouraged the development of other new technologies to treat our patients including shock wave lithotripsy, ureteroscopy, percutaneous renal surgery and laparoscopic approaches to disease of the upper urinary tract. He was particularly supportive of my endeavor to obtain my own percutaneous renal access without help from our colleagues in radiology. He shared my belief that correct percutaneous renal access was the key to successful percutaneous renal surgery, just as appropriate exposure was the key to any open surgical procedure. Our early successes with urologist-obtained renal access undoubtedly contributed to the widespread adoption of the technique and continues to be, 20 years later, one of our most frequently-performed and efficacious stone procedures.
Dr. Tanagho organized our Department around a core of individuals trained in the various subspecialties of urology. This model, virtually unheard of in those days, is now mirrored by academic urology departments around the country. More importantly, Dr. Tanagho emphasized the personal and professional development of the urologists in our Department. He inspired me to constantly strive to be best endourologist I could be, and he insisted every one of us commit to lifelong learning and to continued improvements in the way we care for our patients.“
In the last 35 years, Dr. Tanagho's research has focused on the feasibility of controlling micturition by electrical stimulation of the spinal cord or sacral roots. Identifying the sacral root and implanting tiny electrodes around the autonomic fibers (after isolating them from the somatic fibers) has proved successful in controlling micturition. Neural stimulation has been tested in clinical studies for the FDA in many centers in the states as well as overseas and is now widely used. This work has resulted in eight issued U.S. patents.
Owing to the significance of the neural stimulation research, Dr. Tanagho has been the recipient of the Jacob K. Javits Neurosciences Award for the last 10 years-the only urologist to be so honored. Dr. Tanagho also has been awarded honorary membership in the Urologic Society of Czechoslovakia, the Egyptian Urologic Society, Urologic Society of Australasia, All Union Association of Urology, USSR, German Urological Association, and the Urologic Society of Japan. During these productive years, Dr. Tanagho published more than 300 original articles in peer-reviewed journals and over 120 chapters in urologic texts. He has been the author and editor of seven books and co-editor (with Jack McAninch) of Smith's General Urology since 1988.
Dr. Tanagho was recognized by the late Egyptian President Anwar Sadat, who bestowed on him in 1978 the Decoration of Merit of the First Degree for his valuable contribution to medicine and research.
THE PETER R. CARROLL YEARS
1996 to 2019
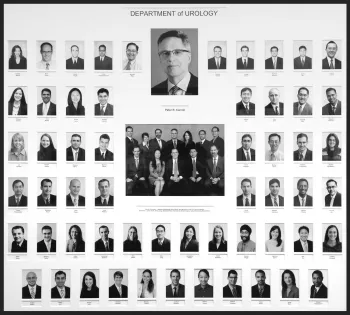
In 1996, Dr. Peter Carroll was appointed chair of the UCSF Department of Urology. Building upon the growth ushered by Dr. Tanagho, Dr. Carroll has led the Department into the 21st century, by vastly expanding the breadth and depth of clinical and research activities. He recruited numerous highly–skilled clinicians, clinician-scientists, and basic scientists, and expanded the department’s research efforts. He recruited the department’s first woman faculty member, and has promoted the entry and advancement of women in urology. During his tenure, there has been an over 3-fold increase in the number of research grants. As a result, the Department currently ranks as one of the very best departments in the country as evidenced by its top-tier ranking by US News and World Reports. It ranks as one of the highest recipients of NIH funding today. During his tenure to date, six endowed chairs within the department have been appointed. Department faculty are clinical and basic research leaders in the field reflecting the spectrum of urologic disorders.
Dr. Carroll continues to focus on developing and expanding the Department’s facilities, growing, diversifying and expanding its research and training programs. As Chair of the Department of Urology, Surgeon-In-Chief of the UCSF Helen Diller Comprehensive Cancer Center; and Associate Dean of the School of Medicine, he fosters an environment where clinical expertise is recruited and nurtured, and promoted. He has led and overseen several capital projects on the UCSF Medical Center Campus, including the Diller Cancer Research Building at UCSF’s new Mission Bay Campus (Figures 6 & 7) He has continued to develop the Urologic Oncology Service, one of the most active multidisciplinary programs, scientifically and clinically, at UCSF.

Figure 6: Dr. Peter Carroll MD, MPH (right) and Van Van Auken (Co-Chair of the Endowment Campaign for UCSF’s Comprehensive Cancer Center)
Signature areas of Dr. Carroll’s research, and one for which he is internationally renowned, is prostate cancer active surveillance, risk assessment and health services research. He pioneered and remains a vocal advocate for standardizing an Active Surveillance regimen in patients with low-burden, early stage prostate cancer. He is committed to reducing the burden of prostate cancer treatment -- physical, psychological and monetary.
In 1995, Dr. Carroll brought the nascent CaPSURETM registry to UCSF. CaPSURETM is a longitudinal, observational study of more than 14,300 men with all stages of biopsy-proven prostate cancer. Patients have enrolled at 43 community urology practices, academic medical centers, and VA hospitals throughout the United States since 1995. Using the clinical data provided by both clinicians and participating patients, CaPSURE™ research findings have expanded knowledge of prostate cancer risk prediction, diagnostic trends, treatment patterns, outcomes and quality of life. CaPSURE™ investigators have published more than 125 articles in peer-reviewed journals and presented over 200 papers at professional conferences. Dr. Carroll continues to serve as its principal investigator, and has expanded its reach to more than 40 sites across the United States.
In addition, Dr. Carroll established the CaPSURE™ Scholars Program in Prostate Cancer Outcomes Research. The goals of this program are to advance prostate cancer research and to support the career development of young investigators at leading institutions across the country. Research topics include clinical outcomes, utilization of health care resources and quality of life. Since 1999, scholarships have been offered to qualified residents and fellows at accredited US training institutions. Scholars, working from their home institutions, formulate research plans under the mentorship of senior CaPSURE™ investigators.
Early in his tenure, Dr. Carroll founded the department’s Urologic Oncology Database, for the purpose of advancing research in bladder, renal, and prostate cancer. Health information is collected at key milestones, cataloging each patient's progress and building a body of knowledge to enhance clinical care. With data from roughly 5,000 participants, the information from consented patients also supports research in the department including biomarker discovery, nutritional epidemiology, novel therapeutics, quality of life and high-risk markers.
Today’s UCSF Urology Training Program
Dr. Carroll also had the foresight to found the department’s Comprehensive Tissue Core. Over 6,000 volunteers have donated bladder, renal and prostate tissue specimens for preserved storage. Dr. Carroll and investigators currently use this resource to determine how biomarkers change over time, what activates them, and what modifiable factors might affect these changes. We have found this tissue core to be increasingly valuable resource as constantly developing advanced research technologies permit new vantages for research.
Peter R. Carroll

Dr. Peter Carroll received his undergraduate training at the University of California, Berkeley. He attended Georgetown University School of Medicine, and during his training, earned the Cahill Award for outstanding performance in surgery, and, the Kober Award for highest record of academic performance. He graduated from Georgetown with honors.
He then came to UCSF for his general surgery training and urology residency. During this time, he earned numerous resident clinical and research awards. He went on to complete a fellowship in Urologic Oncology at Memorial-Sloan Kettering Cancer Center before returning to join the faculty in the Department of Urology at UCSF in 1986.
Throughout his years at UCSF, Dr. Carroll’s contributions to both his department and to the UCSF campus community, are noted for leadership, vision, and a tenacious commitment to clinical care, education, and research at the highest levels. He holds the Ken and Donna Derr-Chevron Distinguished Professorship. He has served as surgeon-in-chief of the UCSF Comprehensive Cancer Center from 2003 through April of 2007. In September 2006, Dr. Carroll became the Director of Strategic Planning and Clinical Services of the UCSF Helen Diller Family Comprehensive Cancer Center and Associate Dean, School of Medicine. In May 2008, Dr. Carroll earned a Master’s in Public Health degree from UC Berkeley. He was awarded the 2010 Eugene Fuller Triennial Prostate Award and the Society of Urologic Oncology (SUO) Medal from the AUA and SUO, respectively.
Dr. Carroll has authored or co-authored over 6500 publications. He is an active member of numerous professional medical societies, including the Alpha Omega Honor Medical Society, the American College of Surgeons, and the American Association of Genitourinary Surgeons. He is now Past President of the American Board of Urology (2006-2008). He is currently principal or co-investigator on numerous scientific studies funded by the NIH.
His major professional interests are the study and management of urologic cancers, Including identifying clinical and pathologic determinants of prostate cancer recurrence, progression, and mortality; discovering novel biomarkers for prostate cancer diagnostics and prognostics; developing evidence-based guidelines for improved management of prostate cancer patients; and examining the impact of lifestyle on health-related quality of life and survivorship among men with prostate cancer. Other interests include innovative methods of urinary tract reconstruction, health services research, health policy and the impact of cancer detection and treatment on quality of life.
Today’s UCSF Urology Training Program
Dr. Carroll has amassed a dedicated team of prominent bench scientists and brought them together with world-class clinical investigators, all of whom share a passionate commitment to translationalresearch. Under Carroll’s leadership, faculty members lead research programs in endourology, laparoscopy and urinary stone disease, male infertility and reproduction, neurourology, male erectile dysfunction, pediatric urology, trauma and reconstructive surgery, tissue regeneration, urology outcomes, incontinence, and urologic oncology.
Currently, the department has over 42 faculty members. Faculty are renowned leaders in the field for several urologic domains: urologic oncology, prostate cancer active surveillance, laparoscopic and robotic surgery, pediatric urology and hypospadias, trauma and reconstruction, erectile dysfunction and penile physiology, Peyronie’s disease, andrology, female urology, stone disease and surgery, and laparoscopic reconstructive urology.
Several current faculty today are supported by NIH mentored clinical and basic research K-awards. Several current members of the department have obtained a Masters in Clinical Research (MAS) degree from UCSF’s prestigious Department of Biostatistics and Epidemiology, and others are active in the UCSF Clinical and Translational Sciences Institute and the latter’s K-scholars program, which provides a organized forum for junior-faculty with K-awards to collaborate, provide peer review, and receive mentorship to advance their academic careers and compete for NIH funding. In 2012, the department ranked among the top recipients of National Institutes of Health research funding for academic urology programs in the U.S.
Residency Training. Three residents enter our six-year program each year. Our residents are culturally and gender diverse. For the last several years, one to two thirds of our incoming resident trainees are women. Until 2011, the first two years of the urology residency program were spent completing general surgery training. As of 2011, residents complete 1 year of general surgery, followed by five years of urology (four years clinical, and 1 year dedicated to research) beginning in the R2 year. Our residents rotate among three main institutions: University of California San Francisco Hospitals (Moffitt Long Hospital and Mt. Zion Comprehensive Cancer Center), San Francisco General Hospital, and the San Francisco Veterans Administration Medical Center.
Under Dr. Carroll’s leadership, our training program’s resident rotations have been re-structured to provide our residents with more a more extended and in-depth exposure to the various subspecialties of urology represented by our faculty. We provide dedicated rotations in the subspecialties of urologic oncology, pediatric urology, urinary stone disease, female urology, erectile dysfunction and sexual medicine, reconstructive urology, male infertility, and neurourology. Our residents today begin training with the DaVinci robot beginning in the R2 year. The fifth year of the residency program continues to be dedicated to research training. Residents may spend the year in a UCSF laboratory performing basic research, or, may focus on clinical and clinical outcomes research. All residents may also complement their research training with clinical research, public health, health policy, and/or epidemiology/biostatistics coursework.
The UCSF Urology Residency training program has over many years hosted many leaders in urology as our annual John Walter Schulte Visiting Professor (Table 2). In addition to training over 240 urologic residents, The UCSF program has trained and supervised more than 174 clinical fellows. This group of scholars includes many from foreign countries: alumni represent over 25 countries, mostly in Europe, South America, Canada and the Far East. Not shown on the table provided are the hundreds of research scholars who have completed research fellowships at UCSF. The research achievements and quality work of these individuals represents a significant contribution to our department’s achievements.
During the near century since its’ founding, and under the successive leadership of Drs. Hinman, Smith, Tanagho, and Carroll, the UCSF Department of Urology has contributed immensely to the urologic literature. Our Chairs and Faculty have always been dedicated to creating an academic environment that encourages a mastery of the foundations of urology, original thought, a humanistic spirit towards medicine and urology, and involvement in research. Over the decades, the Chairs who have led the Department have provided every possible means of support for its members to enhance the productivity of faculty, residents, and fellows. Evidence of this high quality has been reflected in the fact that every junior faculty member has become recognized nationally within a few years of completing training. As Dr. Maurice Garcia, a recent graduate of the residency program and current faculty member reminisces, “From the moment I entered the department as a junior resident, I was struck by how Dr. Carroll consistently, throughout my years of training, promotes, not only an un-flagging pursuit of achievement and distinction among my peers, but also self-development, an open-mind to new research directions, and a fulfilling personal life outside of medicine. For as long as I can remember, outside of his office window, there is a poster called “Peter’s Laws: The creed of the sociopathic obsessive compulsive” While waiting outside of his office to meet with him (usually in the early evening), I was able to read, and eventually nearly memorize all 19 “laws”. The two that most remind me of him and the example he set for us all are #11 (‘Perfection is not optional’), and #17:(‘Patience is a virtue, but persistence to the point of success is a blessing’).”
The result of the department’s productivity is clearly seen in the number of national and international awards the Department has won (see Table 4) and in its contribution to the annual meeting of the Western Section of the AUA. Over the years the UCSF program, while representing only 1 of 14 universities within the Western Section, has contributed close to 20% of the scientific program. It has also won more than its share of the competitive awards offered (Table 5). While the accolades and awards of the department’s basic research faculty and their labs are not enumerated here, their immense contribution to the productivity of the department is acknowledged with pride and gratitude.
Department Clinical Faculty: 2014
(Listed in alphabetical order)
Laurence S. Baskin, M.D.
Dr. Laurence Baskin, MD graduated from the University of California at Berkeley with a Bachelors of Science in Biophysics and attended medical school at UCLA. He then completed two years of general surgery training and a urology residency at UCSF. Dr. Baskin is now a fellowship-trained pediatric urologist, having trained for two years under Dr. John W. Duckett at the Children's Hospital of Philadelphia. Since completing his fellowship in 1993, Dr. Baskin has been on the faculty at UCSF, practicing pediatric urology exclusively.
In 1997, Dr. Baskin was appointed chief of pediatric urology. Dr. Baskin is primary author on over 100 peer-reviewed articles, a dozen invited chapters and is editor of the Handbook of Pediatric Urology. Dr. Baskin is Principal Investigator on basic urologic research funded by the National Institutes of Health. He has also received grants from the National Kidney Foundation, American Foundation for Urologic Disease, and the Academic Senate and Regents Education Fund at UCSF. Dr. Baskin has a specific interest in genital development and reconstructive surgery and has founded the Center for the Treatment and Study of Hypospadias.
Dr. Baskin is an active member of the American Academy of Pediatrics, Society of Pediatric Urology, Past President of the Society of Fetal Urology, current President of the Asian Pacific Association of Pediatric Urology, active member of the American Urological Association and a Fellow of the American College of Surgeons. He was recently elected President of the Society of Pediatric Urology. He received 2010 AUA Foundation John W. Duckett, MD Pediatric Urology Research Excellence Award. Dr. Baskin is especially proud to have participated in humanitarian pediatric urology surgical trips to San Pedro Sula, Honduras and Saigon, Vietnam.
Benjamin N. Breyer, M.D., MAS.
Dr. Benjamin N. Breyer, MD, MAS graduated with a Bachelor of Science from the University of Illinois at Urbana, majoring in Cell and Structural Biology with a minor in Chemistry. Dr. Breyer attended the University of Chicago Pritzker School of Medicine. At graduation, he was elected to the Alpha Omega Alpha honor society, achieved campus wide honors and was given the John Van Prohaska Award for outstanding potential in teaching, research, and clinical medicine.
Dr. Breyer performed two years of general surgery residency at the University of California at San Francisco, where he also completed his urology residency in the Department of Urology and served as Chief Resident. He completed a trauma and reconstruction fellowship under the direction of Dr. Jack W. McAninch. He completed a 2-year master’s degree program in clinical research from UCSF’s Department of Biostatistics and Epidemiology.
Dr. Breyer’s primary research interests involve urologic reconstruction, lower urinary tract disease and sexual medicine. He is currently an NIH career development scholar. He has authored or coauthored over 85 peer-reviewed articles and book chapters. His clinical interests include urethral and penile reconstruction, male fistula repair, men's sexual health, lower urinary tract symptoms and benign prostate surgery, and general urology.
Peter R. Carroll, M.D., MPH.
Dr. Peter Carroll received his undergraduate training at the University of Çalifornia, Berkeley. After graduating with honors from Georgetown University School of Medicine, he came to UCSF for his general surgery training and urology residency. He completed a fellowship in Urologic Oncology at Memorial-Sloan Kettering Cancer Center before returning to join the faculty in the Department of Urology at UCSF.
Dr. Carroll organized the Urologic Oncology Service, one of the most active multidisciplinary programs at UCSF. In 1996, he assumed the chair of the UCSF Department of Urology, consistently ranked as one of the top urology departments in the country by U.S. News and World Report. He holds the Ken and Donna Derr-Chevron Distinguished Professorship, and he has served as surgeon-in-chief of the UCSF Comprehensive Cancer Center from 2003 through April 2007. In September 2006, Dr. Carroll became the Director of Strategic Planning and Clinical Services of the UCSF Helen Diller Family Comprehensive Cancer Center and Associate Dean, School of Medicine. In 2008, Dr. Carroll earned his MPH from UC Berkeley.
Dr. Carroll has authored or co-authored over 400 publications. He is an active member of numerous professional medical societies. He is now Past President of the American Board of Urology (2006-2008). He is currently principal or co-investigator on numerous scientific studies. His major professional interests are the study and management of urologic cancers, innovative methods of urinary tract reconstruction, health services research, health policy, and the impact of cancer detection and treatment on the quality of life.
Dr. Carroll was awarded the 2010 Eugene Fuller Triennial Prostate Award and the SUO Medal from the AUA and SUO, respectively.
Matthew R. Cooperberg, M.D., MPH.
Dr. Matthew Cooperberg, MD, MPH received his undergraduate training from Dartmouth College, where he obtained a degree in English with high honors. He then enrolled in Yale University's MD, MPH program, concurrently earning an MPH with a concentration in Health Policy from the School of Epidemiology and Public Health, and a MD from the School of Medicine in 2000. He completed his General Surgery and Urology training at the University of California San Francisco, and subsequently continued at UCSF to complete a fellowship in Urologic Oncology under the guidance of Peter Carroll, MD, MPH.
In 2009, Dr. Cooperberg was recruited to join the faculty at UCSF and the San Francisco Veterans Affairs Medical Center. Specializing in urologic cancer care, he is part of the multidisciplinary urologic oncology team of the UCSF Helen Diller Family Comprehensive Cancer Center, located at the Mount Zion Medical Center. He also operates at San Francisco General Hospital. Dr. Cooperberg's clinical interests include the diagnosis and management of genitourinary malignancy, and using minimally invasive techniques to treat benign and malignant diseases. He performs robotic, laparoscopic, endoscopic, and percutaneous surgeries, and is interested in incorporating promising new technologies into his practice. Dr. Cooperberg is a candidate member of the American Urological Association (AUA), the Western Section of the AUA, and the American College of Surgeons. He has written over 50 peer-reviewed scientific articles, nine chapters, and presented national and international invited lectures that address benign urologic disease and urologic oncology, with a particular focus on prostate cancer.He was recently awarded the Prostate Cancer Foundation Young Investigator Award.
Hillary Copp, M.D., MS.
Dr. Hillary Copp, MD, MS graduated from the University of California Santa Barbara Summa Cum Laude with a Bachelors of Science in Biology. She attended medical school at Penn State University's College of Medicine. She then completed a one year general surgery internship and a urology residency at the University of Virginia in Charlottesville. This was followed by a fellowship in pediatric urology at Stanford University where she concurrently earned a master's degree in Epidemiology. In 2009 Dr. Copp joined the faculty in the Department of Urology at UCSF as a participant in the multidisciplinary K12 Urologic Research (KURe) Career Development Program.
Dr. Copp has received many awards, as a medical student she received an Alumni Endowed Scholarship and was inducted into the Alpha Omega Alpha National Medical Honor Society. As a resident she received the Merck Achievement of Academic Excellence award, and as a fellow she received a Urologic Diseases in America grant. Dr. Copp’s current research interests are in the areas of health outcomes and the utility of antibiotic prophylaxis in prevention of urinary tract infection in children with hydronephrosis. Dr. Copp is a member of the American Urological Association (AUA) and the American Academy of Pediatrics. She serves as a member on the Pediatric Vesicoureteral Reflux Clinical Guidelines Panel for the AUA, and as a reviewer for the Journal of Urology.
Donna Deng, M.D.
Dr. Donna Deng, MD completed a double major in Molecular & Cell Biology and Classical Civilization as an undergraduate at the University of California, Berkeley. She attended medical school at the University of California, Davis, and received her medical degree in 1998. That same year she received the Loren D. Carlson Student Research Award, which is given to one senior medical student for the best research accomplished during her tenure at the UCD School of Medicine.
Dr. Deng continued her medical education from 1998 through 2004 at the University of California, San Francisco, where she was a resident in urology. In 2001 she was one of three UCSF house-staff elected to the Alpha Omega Alpha Honor Medical Society by the graduating medical class. This honor was given in recognition of her excellence in medical education and patient care. Following her residency, Dr. Deng spent completed her fellowship in pelvic reconstruction and female urology under Sr. Shlomo Raz at the University of California Los Angeles.
Michael DiSandro, M.D.
Dr. Michael DiSandro, MD graduated from Colgate University with a Bachelors of Arts in Chemistry, where he received the Stanton Award for being the top pre-medical student. He attended medical school at University of Vermont College of Medicine. He then completed two years of general surgery training and a urology residency at the University of California, Davis followed by a fellowship at the University of California, San Francisco in pediatric urology under Laurence Baskin, MD, and Barry Kogan, MD. Before returning to join the faculty in the Department of Urology at UCSF, Dr. DiSandro was faculty at the University of Minnesota Medical School and the University of Miami School of Medicine, as well as an attending Pediatric Urologist at the Miami Children's Hospital.
Dr. DiSandro was an American Foundation of Urologic Diseases (AFUD) research scholar and a recipient of a National Institutes of Heath Research Service Grant. He has published numerous journal articles and has won several awards at national meetings, including the James L. Goebel Prize for top research presentation at the Western Section of the American Urological Association meeting. Dr. DiSandro’s current research interests include vesicoureteral reflux, probiotics for urinary tract infection prophylaxis, minimally invasive pediatric urologic surgery, hypospadias and reconstructive urology, and the role of environmental factors in causing hypospadias and other genital anomalies.
Dr. DiSandro is a member of the American Urological Association, the American Medical Association, The Society for Fetal Urology and is a Diplomat of the American Board of Urology.
Maurice Garcia, M.D., MAS.
Dr. Maurice Garcia, MD, MAS received his undergraduate training from the University of California, Berkeley, where he obtained a degree in Psychology. He earned his MD degree from Georgetown University School of Medicine, and completed his residency in urology at UCSF. Following residency, he completed a research and clinical fellowship in Sexual Medicine and Neurourology, under the guidance of Dr. Tom Lue. He completed a 2-year Master’s Degree program in clinical research in UCSF’s Department of Biostatistics and Epidemiology.
Throughout his studies Garcia has pursued in interest in clinical practice, and basic science/clinical translational research. Dr. Garcia’s clinical practice and research focuses are: penile reconstructive surgery, men’s sexual health, erectile dysfunction, Peyronie’s disease, sexual dysfunction, urinary incontinence, voiding dysfunction, and general urology. Other areas of active research include sperm and preimplantation embryo selection for IVF, mobile health technology, and urethral catheter related urethral injury.
In 2008, Garcia was the recipient of a three-year mentored career-development fellowship award to study men’s reproductive health funded through Urology's NIH funded Men's Reproductive Health Research K-12 Program, under the mentorship of Drs. Tom Lue and Peter Carroll. In 2011, as principal investigator, he was awarded an NIH K08 award to continue translational research using a novel technology he co-developed with electrical engineers at UC Berkeley to predict sperm and preimplantation embryo quality, for the purpose of improving IVF outcomes. This work was awarded the AUA’s First Place award for the 2010 AUA Meeting Physician’s Essay Contest.
More recently, Dr. Garcia has also developed a novel fiducial marker and treatment strategy to optimize radiotherapy in the treatment of muscle-invasive bladder cancer, which has been in use for patient treatment at UCSF since 2007. He has also developed a smartphone and social media-based research platform currently in use at UCSF. Together with resident co-inventors from the UCSF Department of Urology, he has designed a urethral catheter design to minimize risk of catheter-balloon urethral injury during both routine placement and traumatic self-removal.
Dr. Garcia is an active member of the American Urological Association, the Engineering in Urology Society, the American Society of Andrology, the International Society of Sexual Medicine, and the Society for Clinical and Translational Science. He has won numerous awards for his research, and has several U.S. Patents issued and pending.
Kirsten Greene, M.D., MAS.
Dr. Kirsten Greene received her undergraduate training from the University of Virginia where she obtained a degree in Interdisciplinary Studies on full academic scholarship. She received her MD from the Johns Hopkins University School of Medicine in May 2000. She then completed her general surgery and urology training at the University of California, San Francisco where she was inducted into the Alpha Omega Alpha Honor Society and received the House Staff Teaching award in 2003.
Dr. Greene combined her interest in urologic oncology, minimally invasive surgery and outcomes research by completing a master's degree in clinical research at the University of California, San Francisco. Dr. Greene specializes in urologic cancers and laparoscopy. She is part of the multidisciplinary urologic oncology team of the UCSF Helen Diller Family Comprehensive Cancer Center located at the Mount Zion Medical Center. She is the Chief of Urology at the San Francisco Veterans Affairs Medical Center.
Dr. Greene’s clinical interests include screening, diagnosis, and management of genitourinary malignancy and minimally invasive treatment of urologic disease. She has experience with robotic, laparoscopic, and endoscopic surgery and is involved in the development of new technologies and the creation of guidelines for care of urologic malignancies. Greene is an active member of the American Urological Association (AUA), the Western Section of the AUA, the Société Internationale d'Urologie, Society of Women in Urology, and the American Medical Association. In 2012, she was appointed Residency Program Director for the UCSF Department of Urology residency training program.
Tom Lue, M.D.
Dr. Tom Lue, MD graduated with highest honors from the Kaohsiung Medical College in Taiwan in 1972. In 1981, after completing his urologic training at Downstate Medical Center in Brooklyn, Dr. Lue was awarded the Valentine Fellowship from the New York Academy of Medicine to study the neurophysiology of the genitourinary tract at the University of California, San Francisco, Department of Urology.
Dr. Lue joined the urology faculty at the University of California, San Francisco in 1982 as a Clinical Instructor of Urology. He is presently Professor of Urology. Dr. Lue has authored or co-authored more than 380 publications and 12 books. His major professional interests are male sexual dysfunction and Peyronie's disease. He is an internationally recognized expert in penile physiology research and an authority in the diagnosis and treatment of male sexual dysfunction.
Dr. Lue's basic science research encompasses development of animal models for research in: penile physiology, hormone deficiency, cavernous nerve injury, diabetes mellitus and hyperlipidemia. His research team discovered the anatomical mechanism of venous compression during penile erection. Dr. Lue's clinical research includes development of diagnostic tests for erectile dysfunction including: the penile injection and stimulation test, a duplex ultrasound test for penile arterial flow, and pharmacologic cavernosography for venous leakage. In 1983 Dr. Lue was one of the first urologists in the country to offer penile injection for patients with erectile dysfunction. He introduced blood gas determination and color duplex ultrasound for the differential diagnosis of various types of priapism.
Dr. Lue's team has made important contributions to basic research and clinical treatment of Peyronie’s disease. He and his associates published the first article implicating TGF beta in the formation of Peyronie’s plaque and developed the first animal model for the study of Peyronie’s disease.
In 1988 Dr. Lue was the recipient of the American Urological Association's Gold Cystoscope Award. The following year, he was the first recipient of the American Foundation of Urologic Disease's, "Most Innovative Research Award." Dr. Lue's research team has won many competitions including first prizes from: the American Urological Association, the Western Section of the American Urological Assoiation, the Urodynamics Society, the International Impotence Society, and the Lapides Essay contest. Dr. Lue was Chair of the International Consultation on Sexual Medicine held in Paris in July 2003, serving as and the lead author of the meeting's proceedings, which were published under the title “Sexual Medicine: Sexual Dysfunctions in Men and Women."
Jack McAninch, M.D.
Dr. Jack McAninch received his undergraduate B.S. degree at the Texas Tech University, a MS degree from the University of Idaho, and his MD degree from the University of Texas Medical Branch where he was an honor graduate and recipient of the Gold Headed Cane Award in recognition as the outstanding graduating senior. He received his general surgery and urology training at Letterman Army Hospital where he was recognized as the outstanding Resident Trainee and received the Robert B. Skelton Award. He is certified by the American Board of Urology and joined the University of California San Francisco (UCSF) faculty in 1977. He currently serves as Chief of Urology at San Francisco General Hospital and Vice Chairman of the Department of Urology.
Dr. McAninch is recognized as a national and international leader in the field of genitourinary trauma and reconstructive surgery. He has directed a highly recognized surgical team that has led the development of numerous new surgical techniques and new management methods in the field. He continues to be a principal investigator for many active research projects. Since 1990, he has trained over 25 fellows in Genitourinary Trauma and Reconstruction.
His textbook, Traumatic and Reconstructive Urology, is a worldwide acclaimed publication. He is an active member of numerous medical societies, including American Urological Association, American College of Surgeons, American Association for the Surgery of Trauma, and Society of International Urology.
In addition, Dr. McAninch has served as President of American Urological Association and American Board of Urology, as well as Regent of American College of Surgeons. In 2010 McAninch received the Ferdinand C. Valentine Medal, awarded by the New York Academy of Medicine for his contributions to the art and science of urology. In 2012, he was awarded the prestigious American College of Surgeons Distinguished Service Award.
Maxwell V. Meng, M.D.
Dr. Maxwell V. Meng, MD received his undergraduate training from Harvard College, where he obtained his degree in biochemical sciences magna cum laude. He then attended the Johns Hopkins School of Medicine where he was inducted into the Alpha Omega Alpha honor society. Dr. Meng obtained his general surgery and urology training at the University of California San Francisco. Subsequently, he combined his interest in urologic oncology and minimally invasive surgery, completing fellowships in both under the guidance of Peter Carroll, MD, MPH and Marshall Stoller, MD.
Upon completion of his fellowships Dr. Meng has continued as UCSF faculty specializing in urologic cancers and laparoscopy. He is part of the multidisciplinary urologic oncology team of the UCSF Helen Diller Family Comprehensive Cancer Center located at the Mount Zion Medical Center. He also operates at the San Francisco Veterans Affairs Medical Center and San Francisco General Hospital.
Dr. Meng's clinical interests include the diagnosis and management of genitourinary malignancy, and minimally invasive treatment of benign and malignant diseases. He has experience with robotic surgery and is actively involved in the development of new technologies. Dr. Meng is an active member of the American Urological Association (AUA), an active member of the Western Section of the AUA, and a candidate member of the American College of Surgeons. Dr. Meng teaches laparoscopic techniques at the UCSF Urologic Laparoscopy course, and he has moderated the laparoscopy session at the Western Section of the AUA. Dr. Meng has written over 50 peer-reviewed publications and 9 chapters covering many aspects of oncology, minimally invasive surgery, and renal trauma.
Ira D. Sharlip, M.D.
Dr. Ira D. Sharlip, MD is a graduate of the University of Pennsylvania where he earned BA and MD degrees. He did his residency and urological training at the Hospital of the University of Pennsylvania, the University of California at San Francisco and the Middlesex Hospital in London, England. He is board certified in both internal medicine and urology. Since 1980 he has had an active private urological surgery practice in San Francisco. Dr. Sharlip has held a variety of faculty appointments in the Department of Urology, currently he serves as Clinical Professor and Senior Physician Diplomate; he sees patients in the Center for Reproductive Health.
Dr. Sharlip is a nationally and internationally recognized authority on urological aspects of male reproductive and sexual medicine. A world leading authority on the microsurgical treatment of male infertility, he has one of the world's largest experiences performing vasectomy reversal. Dr. Sharlip has written and lectured extensively on these and other urological subjects.
Dr. Sharlip provides his time and expertise as a volunteer to national societies and journals. He served as Co-chair of the Male Infertility Best Practice Policy Committee of the American Urological Association (AUA) and he currently chairs the AUA Vasectomy Guideline Committee and the AUA Male Circumcision Task Force. He is both founder and Past President of the Sexual Medicine Society of North America, and Past President of the International Society for Sexual Medicine, these are prestigious academic societies devoted to human sexual function and dysfunction. Dr. Sharlip is Founder and Associate Editor of The Journal of Sexual Medicine and serves as reviewer for many urological journals including the Journal of Urology.
Formerly a Flight Surgeon in the US Army, Dr. Sharlip is a decorated veteran of the Vietnam conflict. He has a keen interest in international medicine, has consulted in hospitals throughout the world, and has volunteered as a physician and surgeon in developing nations including Kenya, Thailand, Vietnam and Iraq. Dr. Sharlip is leading an effort by the AUA to develop a pool of volunteer surgeons to assist the World Health Organization and other international healthcare agencies to provide male circumcision services in sub-Saharan Africa.
Katsuto Shinohara, M.D.
Dr. Katsuto Shinohara, MD is a native of Japan. He attended Yokohama City University School of Medicine and graduated with highest honors. He received three years of general surgery training at Mitsui Memorial Hospital in Tokyo and completed his urology residency at Kitasato University Hospital in Sagamihara, Japan. He came to the United States in 1984 as a urologic oncology fellow at Baylor College of Medicine in Houston, Texas. After completing the fellowship in 1988, he joined the faculty in the UCSF Department of Urology.
Dr. Shinohara is currently Professor of Urology at UCSF and an attending surgeon at the Department of Veterans Affairs Medical Center in San Francisco. He is a faculty member for the UCSF Genitourinary Cancer Epidemiology and Population Science (G-CEPS) program. programHe is an internationally recognized expert in genitourinary diagnostic ultrasound and minimally invasive techniques for the treatment of genitourinary malignancies. He is a member of the American Urological Association, the Japanese Urological Association, and the American Institute of Ultrasound in Medicine.
James Smith, M.D., MS.
Dr. James Smith, MD, MS received his undergraduate training from the University of California, Berkeley, where he obtained a degree in molecular biology with high honors. He then enrolled in The University of California's Joint Medical Program, a partnership between Berkeley's School of Public Health and San Francisco's School of Medicine, where he earned a master's degree in health and medical science in 2000 and a medical degree in 2002. Smith completed his general surgery and urology training at the University of Utah in Salt Lake City, returning to the University of California, San Francisco as an Andrology Fellow in 2007 for advanced clinical and clinical research training in male reproductive and sexual health under the guidance of Tom Lue, MD and Ira Sharlip, MD.
As Director of Male Reproductive Health at UCSF, Dr. Smith directs the multidisciplinary team providing male fertility preservation counseling and treatment, and evaluates and treats men with general fertility problems, low testosterone, erectile dysfunction, Peyronie’s disease, and testicular pain. He specializes in the use of microsurgical vasovasostomy, vasoepididymostomy, sperm retrieval, varicocelectomy, and spermatic cord denervation. His primary research seeks to improve the understanding of clinical, translational, and basic mechanisms of male reproductive biology with particular emphasis on the effect of cancer treatment on male fertility. Dr. Smith is an active member of the American Urological Association, the American Society for Reproductive Medicine, Society of Reproductive Surgeons, Society for Male Reproduction and Urology, and the Sexual Medicine Society of North America.
Marshall Stoller, M.D.
Dr. Marshall Stoller, MD heads UCSF's urinary stone division, which includes endourology and laparoscopy. Stoller graduated from the University of California at Berkeley in 1976 and went to medical school at Baylor College of Medicine in Houston, Texas. Following medical school, he returned to the San Francisco Bay Area, where he was a general surgical intern and resident at UCSF from 1981-1983 and a urology resident from 1983-1985. The following year he was a clinical instructor and research fellow at the University of New South Wales at Prince Henry and Prince of Wales Hospitals in Sydney, Australia. Dr. Stoller returned to UCSF as a chief resident in the Department of Urology, joining the faculty thereafter. He has helped spearhead a comprehensive program in the management of urinary stone disease at UCSF, where the department has utilized and tested a variety of urinary lithotriptors for the Food and Drug Administration.
Dr. Stoller presently operates at Moffitt-Long Hospital, San Francisco General Hospital and the San Francisco Veterans Affairs Medical Center. His practice emphasizes surgical management of urinary stone disease and minimally invasive endourology.
Dr. Stoller has received multiple awards, including grand prize in the annual Lapides Essay Contest in Urodynamic and Neurourology Research. He has received the Distinction in Teaching Award from the Academic Senate at UCSF. Dr. Stoller volunteers his services at the San Francisco Zoo and has consulted on the care of a wide variety of animals, including orangutans, sea lions, raccoons, tigers, African macaques, Jacob rams, lions, elephants, and penguins. Dr. Stoller has multiple issued and pending U.S. patents. Two years ago, Dr. Stoller initiated a presently ongoing collaboration with researchers at the Buck Foundation to develop a novel and promising model for stone disease: the common fruit fly, Drosophila melanogaster. This work has received numerous awards, including First Place in the 2011 Western Section AUA residents essay contest.
LEGEND
Figure 1: Left picture of the present site of the UCSF Medical Center, Medical, Nursing, and Graduate Schools, c. 1900. Right picture of current the UCSF Parnassus Campus.
Figure 2:
Center: Professor and Chair (1915 – 1950), Dr. Frank Hinman
Resident portraits (rows 1-5, right to left): 1. John F. Pruett, Sidney Olson, A. Elmer Belt, D.M. Morison, T.E. Gibson, A.A. Kutzman, R.K. Lee-Brown, A.B. Helper, M.E. Vecki, Oliver W. Butler, Clark M. Johnson. 2. D.A. Charnock, William Manuel, W.A. Carroll, F.L.A. Gonzales, O. Kemper Mohs, John J. Sullivan, Perry A. Bonar, A. Edward Dart. 3. Verne Ross, D.G. Corbett, J Cordonnier, W.K. Murphy, Tracy O. Powell, T. Brent Wayman, Henry M. Weyrauch, Carl Hartwig. 4. Samuel McMahon, R.A. Peterfy, T.E. LeDuc, Donald R. Smith, Robert A. Burns, James Elliot, Joseph Sorkness, H. Harrington, T.T. Nickels, S.H. Harris, R.G. Weaver, Frederick S. Howard. 5. John W. Schulte, Juan Ayginena, Myer Brodkin, Robert E. DeLAval, LeGrand L. Hall, Frank Hinman, Jr., William R. Smart, Kenward O. Babcock, Stanward S. Schmidt, Thad M. McNamara, John R. Barr. ”
Figure 3:
Center: Professor and Chair (1950-1976), Dr. Donald R. Smith
Resident portraits (rows 1-6, right to left): 1. Matthew Marshall, Jr., William F. Boyer, Paul B. Stratte, Richards P. Lyon, Jose Galvez, Jr., Gerald M. Miler, Harry H. Pitts, Kenneth E. Mooslin, Gilbert I. Smith, Philip A. Lahr. 2. Rudolf O. Oppenheimer, Bernard H. Hymel, Herbert S. Brody, Frank deMilt Hill, Edwin R. Roberts, Jr., Revelle Russell, John. C. Huffer, Ronald Tocantins, Mark I. Tobenkin, Donald A. MacDonald. 3. Marvin P. Jassie, Frank. R. Taval, Robert A. Ayers, Alvin B. Rutner, Theodore G. Osius, Clair E. Cox, Leonard Plaine, E. Lee Simmons, Roger B. Goodfriend, Sumner Marshall, James L. Mee, Donald I. VanGiesen, Jerome M. Weiss. 4. Patrick McLin, David Ferguson, Robert Corbett, Joseph Smith, Irving Katz, L. Richard Hayne, A. Warner Dewey, Jr., Dean Packard, Robert Fisher, Gregory G. Fouts, John F. Schmaelzle, Vernon E. Weldon, Norman G. Miller. 5. Eugene V. Cattolica, Allan Moreira, Alan Shapiro, Jack Hagewood, Albert Wood, Herber F. Cronin, Paul Alpert, Harry P. Novick, Byron C. Olson, Donald G. Linker, Kenneth N. Rankin, Nicholas D. Simopoulos, Alfred A. Alekna. 6. Joseph T. Spaulding, Steven M. Rudy, Robert S. Klein, Ira D. Sharlip, Edward J. Collins, Arnold I. Shatz, John P. Heine, Anthony A. Eason, Gary M. Licklider, James R. Palleschi, James B. Karol, Charles N. Glassman, R. Cameron Emmott
Figure 4:
Center: Professor and Chair (1976-1996), Dr. Emil A. Tanagho
Resident portraits (rows 1-6, right to left): 1. Anthony Eason, Gary Linklider, James Palleschi, James Karol, Charles Glassman, R. Cameron Emmot, Stephen Taylor, Lawrence Werboff, John Pearson, Stuart Flechner. 2. Alexios Diamantopoulos, Robert Kahn, John Roberts, Amos Lash, Karl Anderson, Altan Melamud, Hrair-George Mesrobian, Gary Nicolaisen, Peter R. Carroll, Leon Smith-Harrison. 3. Peter Bretan, George Fournier, Charles Terzin, Jason Abber, Wayne Hellstron, Marshall Stoller, Anthony Avalone, Sbaron Mee, Bradley Orvis, Gregory Broderick, Arturo Martinez, Steven Workman. 4. Joseph Presti Jr., Paul Klosterman, Pramjit Chandhoka, Lionel Foster, Carl Thomas, Laurence Baskin, Mark Gasparini, Jonathan Vapnek, Mark St. Lezin, Gregory Marshall, CuNgoc Phan, Sherif Aboseif. 5. Alexander Ingerman, J. Stuart Wolf ,Christopher Evans, Gordon Gluckman, Mantu Gupta, John Connolloy, Farhad Parivar, Joseph Sardina, Benjamin Rhee, Sansern Borirkchanyavat, Regina Hovey, Craig Iriye. 6. Hiep Thieu Nguyen, Kenneth Nitahara, James Chang, Michael Tran, and Hia-Yang Wu.
Figure 5:
Center: Professor and Chair (1996 – Present), Dr. Peter R. Carroll
Resident portraits (rows 1-6, right to left): 1. Nathalie Barnes, Brian Grady, David Nudell, Reza Goharderakhshan, Maxwell Meng, Rodman Rogers, Joseph Franks, Shahram Golami, David Wu, Johnny Chang. 2. Theresa Koppie, Viraj Master, Donna Deng, Rajveer Purohit, Edward Yun, Sean Elliott, Sangtae Park, Nadeem Rahman. 3. Jill Buckley, Kirsten Greene, Thomas Minor, Maurice Garcia, Adam Hittelman, Michael Hsieh, Matthew Cooperberg, Jennifer Mehdizadeh. 4. Surat Phonsombatt, Benjamin N. Breyer, Sean Doyle, Jared Whitson, David Aaronson, Michael Eisenberg, Ephrem Olweny, Thomas Chi. 5. Adam Reese, Gregory Tasian, Sima Porten, Lawrence Flechner, Dana Weiss, Glen Yang, Jacqueline Villalta, Sarah Blashko, Herman Bagga, Catherine Harris, Alex Wu, Lindsay Hampson. 6. Anobel Odisho, Uwais Zaid, Rachel Edlin, Thomas Sanford, Melissa Talbert Sanford
Figure 6:
Dr. Peter Carroll (right) and Van Van Auken (Co-Chair of the Endowment Campaign for UCSF’s Comprehensive Cancer Center) at the groundbreaking ceremony for the Diller Family Cancer Research Center. This 160,000 sq.-ft. laboratory research center is located on the UCSF Mission Bay Campus, which is the future site of UCSF Medical Center
Figure 7:
Dr. Peter Carroll, in the lobby of the Helen Diller Family Cancer Research Building (UCSF Mission Bay Campus), which is home to several department urologic oncology laboratories.
Table 2: John Walter Schulte Visiting Professors
Table 4: UCSF Department of Urology: National and International Awards
Table 5: UCSF Department of Urology: Western Section AUA Awards