Submitted on April 16, 2014
Maurice Garcia, MD, MAS
Assistant Professor of Urology
The U.S. population is, on average, living longer than ever before. As people with chronic diseases live longer, many are presenting with muscle invasive bladder cancer at advanced age, when they are less fit to undergo radical cystectomy (removal of the bladder with urinary diversion using a segment of one's own intestine to either create a urostomy (urine drainage to a urine collection bag at the affixed to the abdominal wall, or, creation of a neobladder (bladder replacement).
An alternative approach to cystectomy, for carefully selected patients, is to maximally resect the tumor (endoscopically) and then treat the the tumor site with high-dose radiation, in combination with chemotherapy. This approach allows the bladder to be preserved. Candidate patients are those whose muscle invasive bladder cancer is localized to the bladder wall, patients with a single tumor focus, and patients who are well informed of the risks and benefits of all treatment options. The approach offers bladder preservation by way of multi-modal treatment: maximal endoscopic tumor resection, followed by combined chemotherapy and radiotherapy.
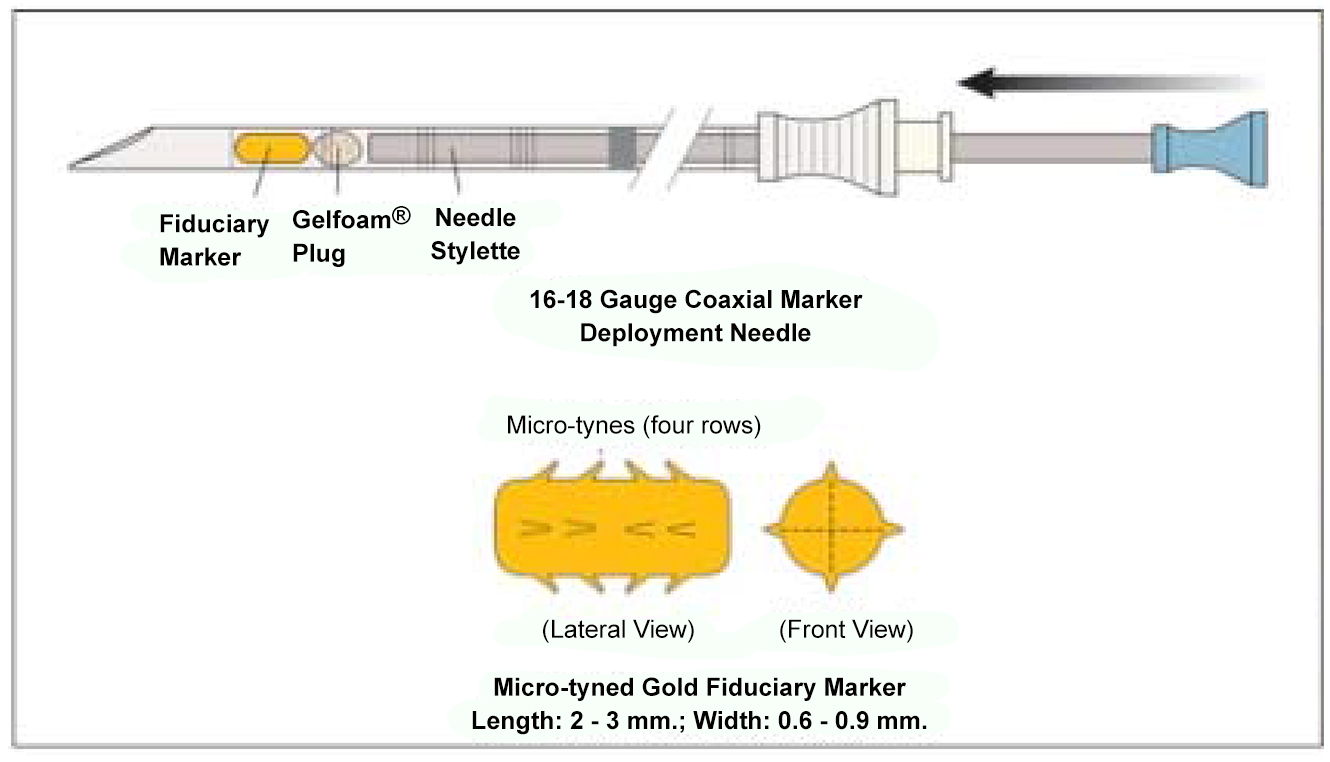
Dr. Maurice Garcia, MD, MAS, Assistant Professor of Urology, UCSF designed and developed an implantable fiducial marker for the bladder that allows Radiation Oncologists to visualize and target the tumor site with high-dosages of radiotherapy, and is spearheading ongoing research to develop their role in clinical treatment.
Modern bladder radiotherapy protocols call for lower-dose radiotherapy to the whole bladder, and higher ("boost") dose to the tumor site. However, targeting the tumor site with high dose radiation has been a longstanding challenge, because the exact location of the tumor resection site is not discernible with available radiographic imaging technologies. Furthermore, to make targeting of the tumor site even more challenging, one must consider that the walls of the bladder are constantly in motion - due to urine filling-volume, bowel dissension, and patient positioning. Hence, even day to day, the actual location of the tumor site on the bladder wall changes location in 3-dimensions.
To date, no reliable fiducial marker for use to guide bladder radiotherapy targeting has existed.

Dr. Garcia produced working prototypes of small micro-tined 24-K gold fiducial markers for delivery into the bladder wall immediately surrounding the tumor resection site via a coaxial needle, and, a placement protocol. Using on-table imaging during radiotherapy delivery, the tumor site could be easily visualized in 3 dimensions (pure gold is highly isodense and easily visible with all imaging modalities). The main benefit with these markers is to be able to increase tumor-site targeting accuracy and decrease collateral high-dose radiation. Placement and subsequent use of the markers during radiotherapy also underscores a key requisite of multi-modal therapy: that the treating urologists and radiation oncologists work closely together throught the arc of the patient's care.
In collaboration with Garcia's GU Oncology colleagues, (Alexander Gottschalk, MD, PhD; Jonathan Brajtbord, MD, Badrinath Konety, MD, MBA, Max Meng, MD; Mack Roach III, MD; Peter R. Carroll, MD, MPH) these markers were placed into 32 patients from UCSF and outside centers. UCSF has applied for US and International patents for the markers and placement protocol.
Garcia has found the marker design to be durable (over 98% of the 150+ markers that have been placed remained in place through the end of radiotherapy) do not appear to migrate after placement, and are safe to place and well-tolerated by patients. An additional benefit of the protocol is that it requires, and has resulted in, close communication between the urologic surgeon and the radiation oncologist during treatment planning (marker placement by the urologist) and delivery (radiotherapy).
The team has also found that these fiducial markers are highly useful for combined use with CyberKnife, a modern 3-dimensional high-dose radiation delivery machine designed to use fixed landmarks (such as our fiducial markers) as radiotherapy field-area treatment boundaries.
Perhaps most exciting is that by providing a reliable visible fixed target for high-dose radiation to the tumor site, it has been possible to cautiously increase radiation treatment-doses, which affords the possibility to explore whether higher, but more safely targeted radiation doses translates to higher muscle-invasive bladder cancer cure rates.
Currently, funded by an NIH KO8 Mentored Clinician Scientist Research Award and a research grant from the American Cancer Society, Garcia is working closely with his colleagues from UCSF Radiation Oncology and Urologic Oncology to gather clinical outcome data for a cohort of patients who have received bladder fiducial markers. Early review of data, however, yields excellent disease-specific survival, with bladder preservation.
Click here for full story in PLOS ONE.