Prostate Cancer Screening Saves Lives. Prostate cancer is by far the most common cancer diagnosed in men in the US. Autopsy studies have shown, among men who live to their 80s, up to half have at least a few cancer cells detectable in the prostate.
Around 1 in 6 men are diagnosed in their lifetimes. Most of these diagnoses are so low risk, they do not matter, and perhaps should not even be called “cancer.” These low risk men most often avoid aggressive treatments, and their treatment side effects, and pursue Active surveillance.
Most men diagnosed with prostate cancer live a normal life span and eventually die of something else. However, because prostate cancer is so common, even the small fraction of cancers that are aggressive amount to the second leading cause of cancer death among men (after lung cancer).
Early prostate cancer typically causes no symptoms, and the only way to catch it early, while it is still confined to the prostate and curable, is screening with a blood test called prostate specific antigen (PSA) test. The purpose of screening—usually done in the context of primary care visits—is to determine when a man should get further testing to determine if a prostate biopsy is recommended.
The higher the PSA, the higher the risk there may be prostate cancer in the body. However, as the name implies, PSA is prostate-specific, not prostate cancer-specific. Other, non-cancer, conditions can also affect the PSA. The most common include:
- Benign prostatic hyperplasia (BPH), or enlargement of the prostate, which is extremely common as men age.
- Prostatitis, or inflammation of the prostate, due to infection or other causes
- Trauma, extensive bike riding, instrumentation, etc.
PSA tends to rise due to benign causes, as men age, so it is more reliable as a cancer screen among younger men (before age 60). Although the “normal” threshold of PSA is often defined at 4.0 ng/ml, among most men it should be much lower than that. The median across the whole population of men up to age 60 is generally less than 1.0 ng/ml.
The digital rectal exam (DRE) is a finger exam of the prostate. It is still often used as a secondary screening test, but identifying a clinically meaningful prostate cancer when the PSA is less than 1.0 ng/ml is extremely uncommon. On the other hand, if the PSA is elevated, or if there are symptoms of urinary obstruction, etc., then DRE is an important part of evaluation, rather than of screening per se.
When to Begin Screening
The recommendation from multidisciplinary experts at UCSF is that most men should begin screening at age 45. Men at higher risk (see below) should begin screening at age 40.
Men at Higher Risk Include:
- Men with a close, male family member (father, brother, uncle) who were diagnosed with prostate cancer, especially if they were diagnosed at a younger age (below 65) and/or died of the cancer.
- Men of West / sub-Saharan African descent
- Men with a known genetic risk for prostate cancer such as the BRCA2 gene mutation. (UCSF has the largest genetic testing center in Northern California. https://www.ucsfhealth.org/clinics/cancer-genetics-and-prevention-progr…)
PSA levels can vary quite a bit. If the PSA is elevated, the test should almost always be repeated a few weeks later to make sure it was not just a “blip.” It’s also important to recognize that medications used for BPH, and for hair loss, including finasteride (Proscar, Propecia) and dutasteride (Avodart) can artificially suppress PSA levels. If you are taking these medications, then the PSA should be effectively doubled to determine when additional testing is needed.
When to consider seeing a Urologist for Prostate Cancer Testing?
- Aged 60 or less and a PSA greater than 2 (or >1 in the presence of high risk factors)
- Aged 61 and older and a PSA greater than 3 (or >1 in the presence of high risk factors)
- A Suspicious Digital Rectal Exam (DRE)
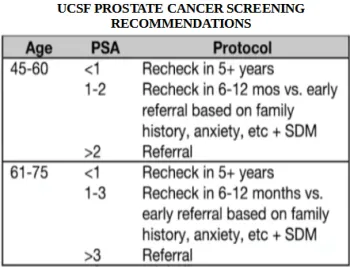
When to Retest PSA? The patient's age and recent PSA test number determine when a man should get another PSA test.
For men aged 40 to 60:
- If the PSA is less than 1.0, recent studies have shown the man has very low risk of being diagnosed with prostate cancer for the next five years. Repeat PSA test every five years or more.
- If the PSA is elevated at 1.0 to 2.0, repeat PSA test every six to twelve months. A Digital Rectal Exam is recommended. Consider referral to a urologist if the man has higher risk or is anxious about the PSA number.
- If the PSA is greater than 2.0, a referral to a urologist is recommended. Note this referral is for evaluation whether or not a prostate biopsy is warranted.
For Men Aged 61 to 75:
- If the PSA is less than 1.0, recheck every five years
- If the PSA is elevated at 1.0 to 3.0, recheck every six to twelve months. A Digital Rectal Exam is recommended. Consider referral to a urologist if the man has higher risk or is anxious about the PSA number.
- If the PSA is greater than 3.0 a referral to a urologist is recommended. Note this referral is for evaluation if a prostate biopsy is warranted. That decision requires further evaluation and testing.
Men Over 75: If the PSA is less than 3, men should discuss with their doctors if further prostate cancer screening can be discontinued.
Life Expectancy Less Than 10 Years: Men with medical conditions that may shorten life expectancy to less than ten years should discuss with their doctors if prostate cancer screening can be safely discontinued.
The above information gives the reader the basic information needed to have an informed conversation with the doctor about the risks and benefits of prostate cancer screening.
| Previous (What is Prostate Cancer?) |