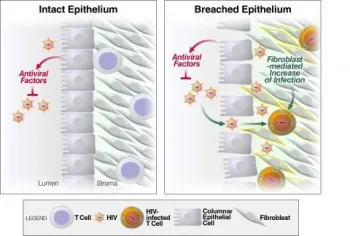
The molecular basis by which small amounts of HIV can initiate infection in the mucosa is not well understood. We have discovered that genital and rectal fibroblasts, amongst the most abundant cells of the mucosa, potently increase HIV infection of T cells. In contrast to fibroblasts, mucosal epithelial cells, which line the mucosa, inhibit HIV infection by apically secreting antiviral factors. Our findings suggest that abrasions in the genital and rectal epithelium may increase HIV transmission in part by allowing HIV to escape an antiviral environment to access the infection-favorable environment of the stromal fibroblasts. Ongoing research in the lab seeks to determine the molecular mechanisms by which stromal fibroblasts increase HIV infection of T cells, and conversely the mechanisms by which mucosal epithelial cells limit infection rates, using ex vivo tissue models. The effects of seminal plasma components, which we previously demonstrated markedly enhance HIV infection, along with sex steroids and microbicide candidates, are also being investigated in these model systems.
- NIH R01 AI127219 “Elucidating the mechanism of progesterone-induced permissivity in the upper female reproductive tract”
- NIH U01 HL146242 "SF Bay Area MACS/WIHS Combined Cohort Study"
- George AF, Neidleman J, Luo X, Frouard J, Elphick N, Yin K, Young KC, Ma T, Andrew AK, Ezeonwumelu IJ, Pedersen JG, Chaillon A, Porrachia M, Woodworth B, Jakobsen MR, Thomas R, Smith DM, Gianella S, Roan NR. Anatomical, subset, and HIV-dependent expression of viral sensors and restriction factors. 2025. Cell Reports.
- Ma T., McGregor M., Giron L.B., Xie G., George A.F., Abdel-Mohsen M.*, Roan N.R.* Single-cell glycomics analysis by CyTOF-Lec reveals glycan features defining cells differentially susceptible to HIV. 2022. *co-corresponding. Elife
- Xie G., Moron-Lopez S., Siegel D.A., Yin K., Polos A., Cohen J., Greenblatt R.M., Tien P.C., Lee S.A., Yukl S.A., Roan N.R. Common and divergent features of T cells from blood, gut, and genital tract of ART-treated HIV+ women. 2022. Journal in Immunology
- Egedal J.H., Xie G., Packard T.A., Laustern A., Neidleman J. Georgiou K., Pillai S., Greene W.C., Jakobsen M.R., Roan N.R. Hyaluronic acid is a negative regulator of mucosal fibroblast-mediated enhancement of HIV infection. 2021. Mucosal Immunology
- Ma T., Luo X., George A., Mukherjee G., Sen N., Sptizer T., Giudice L.C., Greene W.C., Roan N.R. HIV efficiently infects T cells from the endometrium and remodels them to promote systemic viral spread. 2020. ELife
- Neidleman J.A., Chen J.C., Kohgadai N., Müller J.A., Laustsen A., Thavachelvam K., Jang K.S., Stürzel C.M., Jones J.J., Ochsenbauer C., Chitre A., Somsouk M., Garcia M.M., Smith J.F., Greenblatt R.M., Münch J., Jakobsen M.R., Giudice L.C., Greene W.C., Roan N.R. Mucosal stromal fibroblasts markedly enhance HIV infection of CD4+ T cells. 2017. PLOS Pathogens
- Roan N.R. and Münch J. Improving preclinical models of HIV microbicide efficacy. 2015. Trends in Microbiology
- Zirafi O.*, Kim K.A.*, Roan N.R.*, Kluge S.F., Müller J.A., Jiang S., Mayer B., Greene W.C., Kirchhoff F., Münch J. *Authors contributed equally to work. Semen enhances HIV infectivity and impairs the antiviral efficacy of microbicides. 2014. Science Translational Medicine
- Roan N.R., Liu H., Usmani S.M., Neidleman J., Müller A.J., Avila-Herrera A., Gawanbacht A., Zirafi O., Chu S., Dong M., Kumar S.T., Smith J.F., Pollard K.S., Fändrich M., Kirchhoff F., Münch J., Witkowska H.E., Greene W.C. Liquefaction of semen generates and later degrades a conserved semenogelin peptide that enhances HIV infection. 2014. Journal of Virology
- Roan N.R., Müller A.J., Liu H., Chu S., Arnold F., Stürzel C., Walther P., Dong M., Witkowski, E., Kirchhoff, F., Münch J., Greene, W.C. Peptides released by physiological cleavage of semen coagulum proteins form amyloids that enhance HIV infection. 2011. Cell Host and Microbe